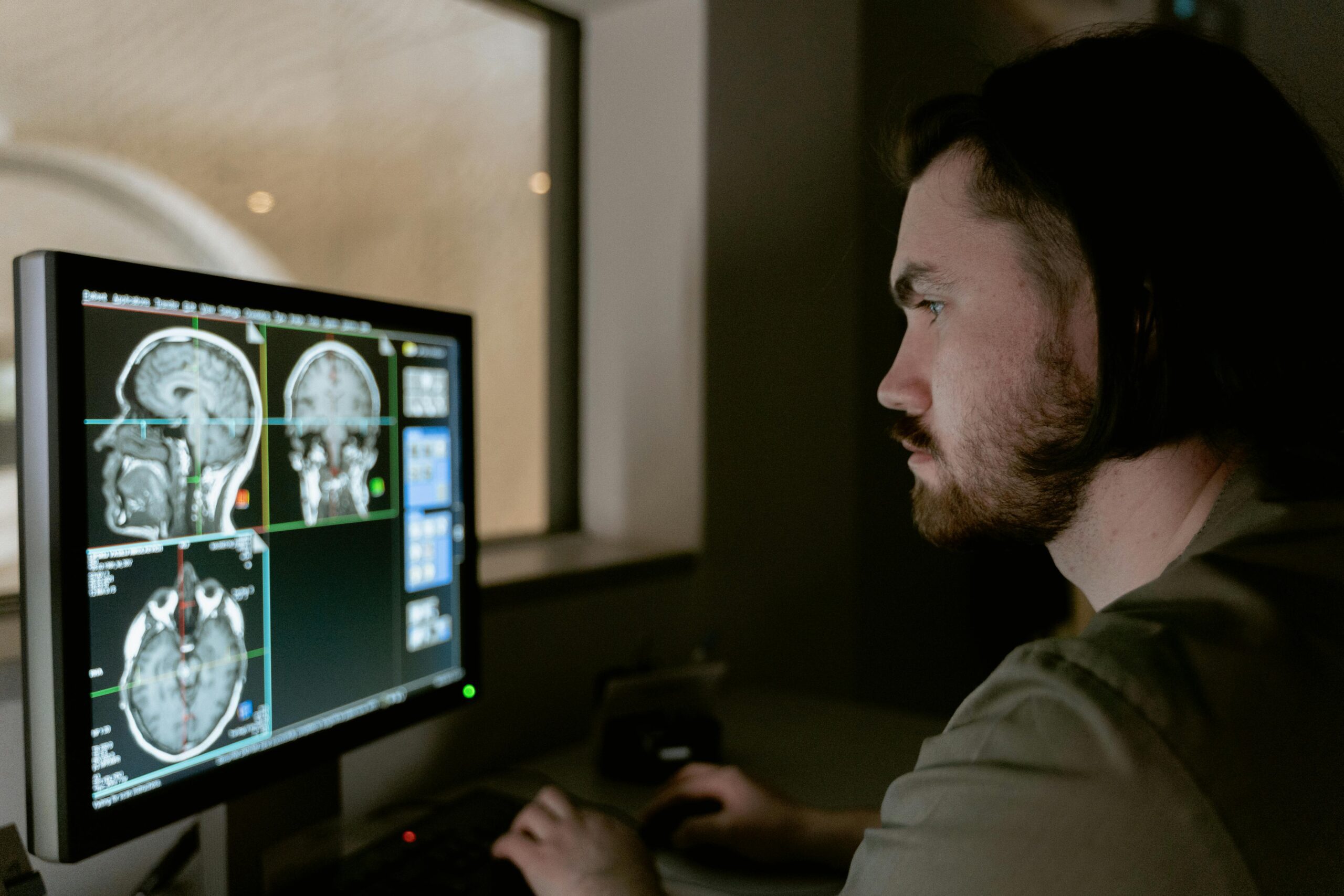
Diffusion Tensor Imaging (DTI) stands at the forefront of MRI technology, revolutionizing the approach to diagnosing, understanding, and treating Traumatic Brain Injury (TBI). This advanced technique tracks the diffusion of water molecules in the brain’s white matter. It offers unparalleled insights into the structural integrity of axons. The use of DTI in TBI cases has become increasingly vital. It enhances diagnostic precision, deepens our comprehension of the injury’s underlying mechanisms, and informs more tailored rehabilitation strategies. This article explores the impact of DTI in the context of TBI. In addition, it emphasizes its contributions to diagnostics and the elucidation of pathophysiology. Furthermore, DTI guides the treatment and recovery processes.
Origins and Development
The theoretical foundation of DTI lies in the work on diffusion MRI. The work began in the 1960s, with early experiments aimed at measuring the diffusion of water molecules in tissues. However, it wasn’t until the late 1980s and early 1990s that researchers began to explore the anisotropic nature of water diffusion in the brain—meaning that water molecules tend to diffuse more easily along the length of nerve fibers (axons) than across them. This anisotropic diffusion is particularly pronounced in the brain’s white matter, where axons are bundled into tracts, making it possible to infer the orientation and integrity of these tracts.
In 1994, Peter Basser and colleagues published a seminal work introducing the tensor model to analyze diffusion MRI data, laying the groundwork for what would become known as Diffusion Tensor Imaging. The tensor model allows for a more comprehensive characterization of the diffusion process, considering the directionality and magnitude of diffusion in three-dimensional space. This critical advancement enables the visualization and quantification of the complex architecture of white matter fibers in the brain. It is crucial for understanding normal brain function and the impact of various neurological disorders.
Advancements and Applications
After its introduction, DTI quickly became a powerful tool in neuroscience research and clinical neurology. Its ability to map the brain’s white matter pathways noninvasively has contributed significantly to our understanding of brain connectivity. It has been instrumental in studying various neurological conditions, including multiple sclerosis, stroke, Alzheimer’s disease, and traumatic brain injury. Additionally, DTI is used to investigate the development and aging of the brain, providing insights into how white matter structures change over the lifespan.
One key application of DTI is neurosurgery, which is used for preoperative planning by mapping out critical brain pathways that must be avoided during procedures. In cognitive neuroscience, DTI has facilitated studying the relationship between brain structure and function, particularly in understanding how disruptions in white matter connectivity relate to cognitive deficits and psychiatric disorders.
Enhancing Diagnostic Precision
Traditional imaging techniques often fail to detect the microstructural changes characteristic of diffuse axonal injury (DAI). Diffuse axonal injury is a prevalent form of damage in TBI. DTI excels where these methods falter in identifying DAI. Visualizing the brain’s white matter tracts and pinpointing areas where axonal damage has altered the diffusion of water molecules. This capability allows clinicians to identify and quantify brain injuries with a level of precision previously unattainable, enabling the formulation of targeted treatment plans.
Deepening Understanding of TBI Pathophysiology
Beyond its diagnostic capabilities, DTI offers a window into the complex pathophysiology of TBI. By mapping out the integrity of white matter tracts, this imaging technique sheds light on the extent of axonal loss and demyelination, contributing to a more nuanced understanding of how TBIs unfold and progress. DTI’s ability to track changes in the brain over time also provides invaluable insights into the injury’s natural history and the impact of various therapeutic interventions, enhancing our comprehension of TBI’s intricate dynamics.
Informing Treatment and Rehabilitation
DTI’s detailed visualization of brain structure and pathology is crucial in personalizing treatment and rehabilitation efforts for TBI patients. Identifying specific areas of white matter damage enables clinicians to tailor rehabilitation programs to individual needs, focusing on recovering functions most affected by the injury. Furthermore, DTI can monitor the brain’s structural changes in response to rehabilitation, offering objective data to refine and optimize therapeutic strategies, ensuring that patients receive the most effective interventions for their recovery.
Navigating Challenges and Looking Forward
Despite the profound advantages DTI brings to TBI care, challenges such as the need for specialized expertise for data interpretation and sensitivity to motion artifacts persist. Additionally, the diverse nature of TBI complicates the standardization of DTI metrics and protocols.
Despite its significant contributions, DTI is not without limitations. The technique can be sensitive to motion artifacts and assumes a simplified water diffusion model. DTI may not fully capture the complexity of brain tissue microstructure. Moreover, crossing fibers within a voxel (the smallest unit of measurement in MRI) can complicate the interpretation of DTI data.
Ongoing research is focused on addressing these challenges through the development of advanced diffusion imaging techniques, such as high angular resolution diffusion imaging (HARDI) and diffusion kurtosis imaging (DKI), which aim to provide more accurate and detailed representations of the brain’s microstructure. Additionally, there is a growing interest in combining DTI with other imaging modalities and big data analytics to deepen our understanding of the brain’s structural and functional networks.
However, ongoing improvements in DTI technology and analysis are steadily overcoming these obstacles, expanding its applications and enhancing its utility in neuroimaging.
Conclusion
Diffusion Tensor Imaging (DTI) dramatically transforms the landscape of TBI management. DTI enables more accurate diagnoses, enriches our understanding of the injury’s pathophysiology, and guides more personalized approaches to treatment and rehabilitation. In addition, as DTI continues to evolve, its role in enhancing the outcomes and quality of life for TBI patients is set to grow, marking a new era in the care and recovery of individuals with traumatic brain injuries.
References
Ranzenberger LR, M Das J, Snyder T. Diffusion Tensor Imaging. In: StatPearls. Treasure Island (FL): StatPearls Publishing; November 12, 2023. https://pubmed.ncbi.nlm.nih.gov/30726046/
Hulkower MB, Poliak DB, Rosenbaum SB, Zimmerman ME, Lipton ML. A decade of DTI in traumatic brain injury: 10 years and 100 articles later. AJNR Am J Neuroradiol. 2013;34(11):2064-2074. doi:10.3174/ajnr.A3395 https://www.ajnr.org/content/34/11/2064
Sotak CH. The Role Of Diffusion Tensor Imaging In The Evaluation of Ischemic Brain Injury – A Review. NMR Biomed. 2002;15(7-8):561-569. doi:10.1002/nbm.786 https://doi.org/10.1002/nbm.786
Bashir U, Yap J, Rasuli B, et al. Diffusion-weighted imaging. Reference article, Radiopaedia.org (Accessed on 10 Mar 2024) https://doi.org/10.53347/rID-16718, https://radiopaedia.org/articles/16718
Andrew J. Steven, Jiachen Zhuo, and Elias R. Melhem, 2013, American Journal of Roentgenology, Volume 202, Issue 1, Diffusion Kurtosis Imaging: An Emerging Technique for Evaluating the Microstructural Environment of the Brain, https://doi.org/10.2214/AJR.13.1136
Diffusion tensor imaging during recovery from severe traumatic brain injury and relation to clinical outcome: a longitudinal study.
Sidaros A, Engberg AW, Sidaros K, Liptrot MG, Herning M, Petersen P, Paulson OB, Jernigan TL, Rostrup E.
Brain. 2008 Feb;131(Pt 2):559-72. doi: 10.1093/brain/awm294. Epub 2007 Dec 14.
PMID: 18083753 https://pubmed.ncbi.nlm.nih.gov/18083753/